January and February were very long months – unable to see family and friends, and stuck at home with nowhere to go. Lots to do though.
The first job to get done was to have our bathroom reconfigured, replacing our old ‘step to enter’ shower with a wider, level access shower suitable for eventual use with a shower wheelchair. Ironic that we could have the skilled plumbers working in our house for two weeks, yet our family members hadn’t been able to visit for months.
We also had visits from the local physiotherapy and occupational therapy teams. Brilliant support from both, although I’m still not fully sure where the boundary lies between their responsibilities. However, the result was the delivery of a brand new four wheel rollator, a new, sturdy walking stick, supportive collars for my aching neck, a set of tailored exercises, raised toilet seats, and a brand new profiling ‘hospital’ bed for my newly designated ‘study bedroom’. I was also measured up for a rise and recline chair and a power wheelchair.
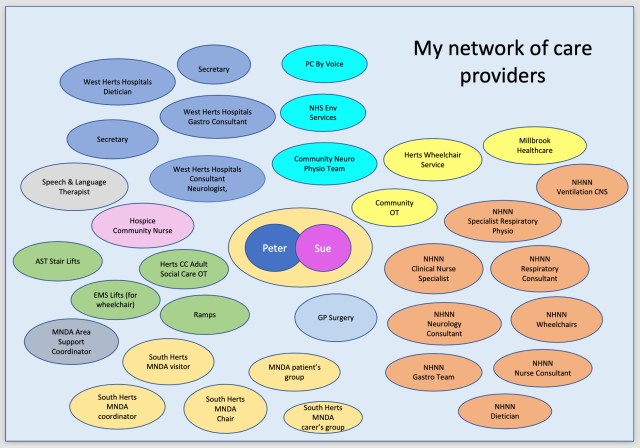
It’s evident that I’m being talked about in case review meeting by the speech and language therapist, physiotherapist, occupational therapist, and the community nurse from the Peace Hospice in Watford. At first glance the various services don’t appear to be joined up to the patient because there are so many people to deal with, but there’s plenty of evidence of information sharing and co-ordination.
In terms of MND progression during this time, I experienced a noticeable loss of function in my right hand and arm, which was quickly catching up with my left. This meant I could no longer get dry when getting out of the shower and could no longer get dressed. This put more pressure on Sue who was having to do more and more. Above all, the worst developing symptom was exhaustion – extreme tiredness after a shower, after getting dressed, after anything really.