Videofluoroscopy
After a negative COVID test, I had a videofluoroscopy examination on 19 October arranged by the Speech & Language Therapist. We shared a concern about my swallowing, and the test would show the extent of the problem. It was a very easy test – you sit in a chair with an X-Ray camera to the side and a large TV screen in front. You then are given a series of different things to eat and drink either coated with, or mixed with, a small amount of barium. On the TV screen I could see my head, mouth and swallowing action with the various samples. I’ve always hated the taste of banana and a coating of barium didn’t enhance the experience!
The result of the test was clear evidence that there was ‘airway penetration’ when I swallowed ‘thin’ liquids like water and tea. In other words, it might be easy for me to get a chest infection from some liquids entering my lungs. There wasn’t a problem with thicker drinks. Crunchy biscuit also caused problems of a tickle in the throat, a cough and the risk of choking.
I was prescribed Resource Thicken Up Clear to add to all drinks in future – for example two scoops in a mug of tea or a glass of water or wine. Thickened wine may sound like a travesty, but the slightly jelly-like consistency is actually very nice. Subsequently I have found that naturally ‘thicker’ drinks (like a cappuccino or flat white), or fizzy drinks (like lager) are not so much of a problem.
MND Association
We made contact with the MNDA in a number of ways. I’d already been looking at their online forum on the website, and I’d looked through many of the really valuable pages of online information. The resources are really good.
We ‘met’ our MNDA Area Support Co-ordinator on a Zoom call, and the local South Herts branch of the association made contact with us. We were in abnormal times during the COVID pandemic, but the local branch organises monthly Zoom calls for carers (which Sue always attends) and also monthly Zoom calls for people with MND. I attend this one less regularly as my speech isn’t great and I find it difficult to participate.
We also were introduced to our really supportive MNDA ‘visitor’ who is in regular contact. She wasn’t able to visit us due to COVID restrictions but monthly phone conversations have been much appreciated, and she is always available to take a call if we have questions or concerns.
Quotes for ‘through the floor’ lifts
There’ll be a specific page in this blog about wheelchairs and lifts, but during October we had various sales people around to provide quotes for through a through the floor lift to would take me in a power wheelchair from our dining room to my newly designated study bedroom above. These lifts are expensive, but much cheaper (in our case) than an alternative option of converting our well used garage into a bedroom and new bathroom. We did have a quote for one very nice looking lift that, on close inspection, was not actually big enough to accommodate a power wheelchair. We could have made a very expensive mistake, as others have done.
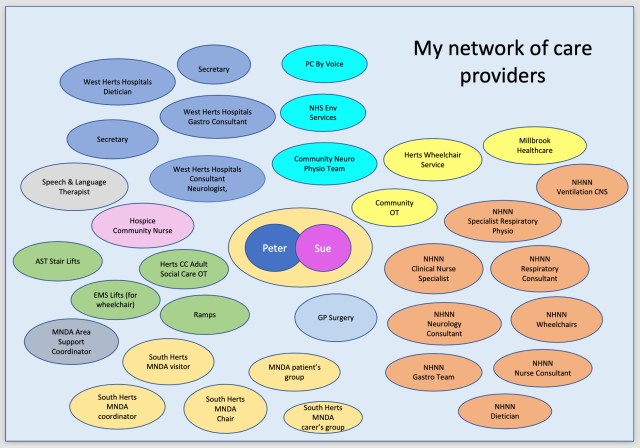
Network of care providers
Towards the end of October we were getting quite confused by all the names, so we started drawing a map of all the people we were having regular contact with, providing us with care and support. You can see how complex the network has become!